| |
Decades of research on
cancer
and
obesity
have established that obesity is one of the greatest risk factors for the development of a variety of cancers including breast, colon and pancreatic cancer. Despite significant advances in cancer treatment and prevention, how or why obesity increases cancer risk still remains unclear. Recent research by Dr. Jian-Wei Gu of the University of Mississippi Medical Center, however, reveals a new connection between the two that could have significant implications for both diseases.
Obesity and Cancer - A Connection
As previous research by Dr. Gu and other scientists has found, fat cells and cancer cells are actually quite similar in their desperate need to receive vital nutrients, particularly oxygen, from the body. These nutrients are delivered to all cells through blood vessels that carry fresh blood from the heart to the rest of the body and back.
As new cells grow and multiply, they require more and more blood vessels to connect them to the network of blood vessels already in place. To stimulate the production of new blood vessels, these cells release a variety of compounds known as angiogenic factors. Any cell that is not receiving enough oxygen, which is carried in the blood, will release these factors. These factors are carried through the blood stream and bind to receptors on cells lining the blood vessel walls, called
endothelial cells.
The binding of angiogenic factors to cell receptors promotes a process called
angiogenesis,
which eventually results in new blood vessels.
New blood vessels can carry more blood and oxygen to the needy cells. The most important regulator of angiogenesis is the angiogenic factor called Vascular Endothelial Growth Factor, or VEGF for short.
Crystal structure of one of the forms of VEGF, from snake venom
As we said before, all cells will release these angiogenic factors to produce new blood vessels when they are in need of oxygen. This is no less true of cancer cells or fat cells.
Fat Cells and Lean Cells
Fat cells are very large in comparison to all other cells in the body (known collectively as lean cells), yet they receive the same amount of blood and oxygen as lean cells. As a result, they are always in a state of low oxygen, known as
hypoxia,
and are thus constantly releasing angiogenic factors to stimulate more blood vessels. Similarly, as cancer cells grow and multiply, they too release angiogenic factors into the blood stream to promote blood vessel growth.

Diet affects the amount of visceral fat in >60 week old female mice.
Top panel: Visceral fat of mice fed a regular diet. Bottom panel: Visceral fat of mice fed a high fat diet.
If it were possible to inhibit this process of angiogenesis, however, it might be possible to inhibit cancer growth and promote weight loss. This was the hypothesis Dr. Jian-Wei Gu and colleagues at the University of Mississippi Medical Center sought to test.
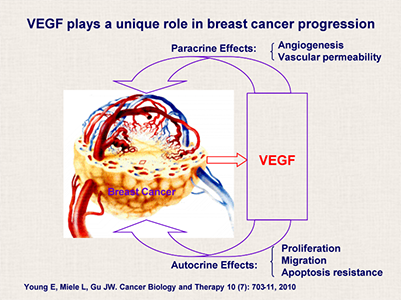
Dr. Gu's hypothesis: breast cancer stimulates VEGF production which feeds back on the cancer cell to cause various effects.
Prior research on cancer conducted by Dr. Judah Folkman, Dr. Donald Ingber, and Dr. Ofra Benny at Harvard Medical School focused on the development of a therapeutic drug to inhibit angiogenesis in cancer cells based on a fungus the researchers had observed to prevent tumor growth. This was the topic of the What A Year article 'A Series of Fortunate Events' published in 2008. In his research, Dr. Gu has extended the work of his Harvard colleagues and other researchers by linking angiogenesis with both cancer and obesity. His experiments seek to determine whether angiogenesis might be inhibited by preventing VEGF from binding to its receptors on endothelial cells that line the walls of blood vessels.
Obese Mice and Mice with Cancer
In an initial series of experiments, Dr. Gu measured the levels of VEGF in the bloodstream of obese mice, mice with breast tumors, and control mice. He found that both obese mice and mice with breast tumors had increased levels of VEGF in their bloodstream when compared to control mice. Next, Dr. Gu and colleagues performed experiments to determine whether it was possible to reduce obesity and tumor growth by inhibiting angiogenesis.
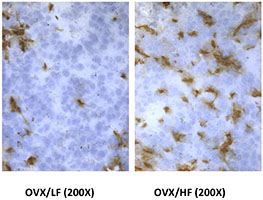
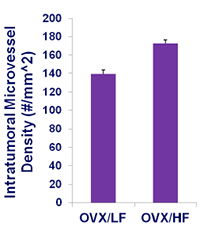
Bigger tumors are associated with more blood vessels
(which is indicated by the red stain on right side of picture labeled OVX/HF)
compared to the mice fed a low fat diet (left side labeled OVX/LF).
In one set of experiments, Dr. Gu used the drug Sunitinib, a known inhibitor of angiogenesis. The researchers found that obese mice treated with Sunitinib had significantly reduced body weight and fat mass than the control mice. In a second set of experiments, Dr. Gu performed similar studies on mice with breast cancer using Sunitinib. The researchers found that Sunitinib significantly inhibited tumor growth in the breast cancer mice when compared to the controls. Sunitinib worked by blocking angiogenesis in the cancer cells. These findings provided evidence that drugs such as Sunitinib could inhibit angiogenesis and be effective treatments to promote weight loss and reduce cancerous growths.
Two Conditions Together
In his most recent research, Dr. Gu has combined his work to include both obesity and breast cancer in a single model. These experiments compared obese mice with cancer to obese mice without cancer and non-obese mice with cancer. The researchers measured tumor weight, tumor angiogenesis, and levels of VEGF in the bloodstream and fat tissue. They found that tumor weight and tumor blood vessel mass were significantly greater in obese mice than non-obese mice. In addition, obese mice without cancer and non-obese mice with cancer had elevated levels of VEGF in the bloodstream compared to their non-obese or non-cancerous counterparts. Obese mice with breast tumors had the highest levels of VEGF, more than obese mice without cancer and non-obese mice with cancer.
"This research allows us to further connect the dots between cancer and obesity."
These results suggested that elevated levels of VEGF in obese mice might be a potential mechanism for the development of cancer. "This research allows us to further connect the dots between cancer and obesity," explains Dr. Gu.
Like the mice in this study, obese people have abnormally high numbers of fat cells and therefore elevated levels of angiogenic factors released into the bloodstream. Dr. Gu hypothesizes that these elevated levels of angiogenic factors may provide a better environment for cancerous growth because the blood vessels cancer cells need to survive are already growing at an increased rate.
These findings have important implications for the treatment of both cancer and obesity. As Dr. Gu found in his first set of experiments, angiogenesis inhibitors could provide a novel therapy for severely obese people. Currently, Sunitinib is approved by the Food and Drug Administration to treat renal cell carcinoma and imitinib-resistant gastrointestinal stromal tumor. In future experiments, Dr. Gu would like to conduct similar research on the effectiveness of angiogenesis inhibitors on tumor growth as well.
Dr. Jian-Wei Gu is an Assistant professor of Physiology at the University of Mississippi Medical Center. He has spent his career studying the process of angiogenesis and its relationship to cancer, obesity, alcohol, exercise, and nutrition, among other biological processes. When not in the laboratory, Dr. Gu enjoys gardening, reading, watching movies and exercising.
For More Information:
- Gu JW et al. 2011. "Postmenopausal obesity promotes tumor angiogenesis and breast cancer progression in mice. Cancer Biology & Therapy, 11(10): 910-917.
- Young E et al. 2010. "SU11248, a selective tyrosine kinases inhibitor suppresses breast tumor angiogenesis and growth via targeting both tumor vasculature and breast cancer cells."" Cancer Biology & Therapy 10: 703-711.
- 3. Gu JW et al. 2009. "Oral administration of pyrrolidinedithiocarbamate (PDTC) inhibits VEGF expression, tumor angiogenesis and growth of breast cancer in female mice." Cancer Biology & Therapy 8: 541-551.
- Gu JW et al. 2013. "Angiogenesis inhibitor, Sunitinib significantly reduces adipose tissue mass in high fat diet-induced postmenopausal obese mice." FASEB J 27:1154.9
To Learn More:
Angiogenesis
- Angiogenesis Foundation. http://www.angio.org/ua.php
- Understanding Cancer: Angiogenesis. National Cancer Institute. http://www.cancer.gov/cancertopics/understandingcancer/angiogenesis
Obesity
- Centers for Disease Control and Prevention.http://www.cdc.gov/obesity/
- World Health Organization. http://www.who.int/topics/obesity/en/recognize.html
- "Obesity in America." The Endocrine Society. http://obesityinamerica.org/
Cancer and Obesity
- "Obesity and Cancer Risk." The National Cancer Institute. http://www.cancer.gov/cancertopics/factsheet/Risk/obesity
- "The obesity-cancer connection, and what we can do about it." American Cancer Society. http://www.cancer.org/cancer/news/expertvoices/post/2013/02/28/the-obesity-cancer-connection-and-what-we-can-do-about-it.aspx
Written by Rebecca Kranz with Andrea Gwosdow, PhD at www.gwosdow.com
HOME | ABOUT | ARCHIVES | TEACHERS | LINKS | CONTACT
All content on this site is © Massachusetts
Society for Medical Research or others. Please read our copyright
statement — it is important. |
|
|
Dr. Jian-Wei Gu

From left to right: Simi Chawla, Jeremy Wells, Emily Young, Dr. Jian-Wei Gu, and Kevan Tucker
Great Science Sites
NIH | High School
NIH | Middle School
ACS | Science for Kids
SciAm | Blog
Sign Up for our Monthly Announcement!
...or  subscribe to all of our stories! subscribe to all of our stories!

What A Year! is a project of the Massachusetts
Society for Medical Research.
|
|

